Cornwall’s ambulance waiting times for strokes 9.9 times longer than national targets
Long delays could have "devastating" consequences for those in need of treatment
Image: Alice Colvin-Cousley
Disclaimer: You should always call 999 in a medical or mental health emergency. This is when someone is seriously ill or injured and their life is at risk.
Ambulance response times in Cornwall for victims of strokes and heart attacks are almost ten times longer than national targets, The Cornish Echo has found.
In September this year, the average wait time for Category 2 calls in Cornwall was two hours and 58 minutes, according to figures provided by NHS Cornwall and Isles of Scilly Integrated Care Board.
These Category 2 calls are for people who are suffering from conditions such as heart attacks, strokes, sepsis or major burns.
National targets dictate that all ambulance trusts should respond to Category 2 calls in 18 minutes on average - meaning response times in Cornwall are 9.9 times higher than the targets.
And Category 1 calls, which are for situations that are classified as life-threatening and needing immediate intervention and/or resuscitation, e.g. cardiac or respiratory arrest, also fell short.
In September this year, the mean figure in Cornwall for a Category 1 call was 15 minutes 48 seconds. This is compared to a national target of seven minutes on average.
A group of clinicians, researchers and campaigners have told The Cornish Echo that the delays could have potentially devastating consequences for those in need of treatment.
“Every minute a stroke is left untreated, 1.9 million brain cells can die,” Jacqui Cuthbert, the Stroke Association’s associate director for the South West and Channel Islands, said.
“The later treatment happens, the harder recovery can be for survivors and the more likely it is that they will be left with severe effects of stroke, including increased disability. Emergency response times are far too long for stroke patients.”
Dr Sonya Babu-Narayan, associate medical director at the British Heart Foundation and consultant cardiologist told The Cornish Echo that ambulance delays matter because minutes can be the difference between “life and death” for heart attacks.
“We know the current workforce can’t do any more than they already are, but despite this, too many people are experiencing extreme waits for ambulances.
“These delays may be leading to people needlessly dying because they couldn’t get lifesaving treatment in time, while others may be left with avoidable heart failure and disability.”
Short time window for stroke treatment
The Stroke Association’s Jacqui Cuthbert told The Cornish Echo that “unprecedented system-wide pressures” are now compromising ambulance response and hospital treatment times, which can have “devastating impacts” for people experiencing a stroke.
The Cornish Echo asked a specialist in emergency medicine to understand what the ambulance delays might mean for patients.
Dr James Gagg, South West regional chair for the Royal College of Emergency Medicine, explained that long ambulance response times could limit the types of treatments patients receive.
Ischaemic strokes, which are the most common type of stroke according to the NHS, can often be treated using injections of a medicine called alteplase, which dissolves blood clots and restores blood flow to the brain.
This use of this “clot-busting” medicine is known as thrombolysis.
“From someone calling for an ambulance, to getting to hospital, they have to have a CT scan and a clinical assessment and then the drugs administered,” said Gagg.
“All of that has to occur within four and a half hours… So the initial part of making a phone call and being conveyed to hospital is a critical element.”
He added that hospitals have procedures to make sure people suffering from stroke are prioritised when they arrive.
While Cornwall’s average waiting time of two hours and 58 minutes would enable people to reach the hospital ahead of the four and a half hour mark, it would leave a shorter window for them to be assessed and receive treatment.
And there have been reports of potential stroke victims waiting in excess of the September average Category 2 time of two hours and 58 minutes.
This September, ITV wrote about a 75-year-old man who had to wait nine-hours for an ambulance after he suffered a suspected stroke.
And an inquest was held this year following the death of a holidaymaker called Anthony James Reedman, who had to wait for nearly three hours for an ambulance to arrive after he suffered a stroke in 2021.
Improved outcomes
Gagg told The Cornish Echo that 10% of patients who are treated with thrombolysis, will survive and live independently as a result of the treatment.
For those who are unable to receive thrombolysis, health outcomes can be affected.
“The risk is that your stroke will leave you with a permanent disability. The extent of that will depend on what the symptoms of stroke are in the first place. Some people with the right rehab and so forth, will have an element of recovery from this,” he said.
“But that recovery may not be to the extent that it would have been if they were able to have this treatment in the first instance. For some patients, they will have a full recovery if they have the treatment, but they'll be left with a disability if they don't.”
Gagg said while the majority of patients who have a stroke won't die, some will.
“It might be that that time critical intervention might have made the difference in some cases.”
He also explained there are some types of stroke where patients are transferred to another hospital, to have a thrombectomy - a procedure where the blood clot is removed.
“That's another aspect of this which needs timely intervention and it can often also require secondary ambulance transfers, which may themselves be delayed. So that adds other layers of risk into this as well - that's for a much smaller proportion of patients,” Gagg added.
Treatment for STEMI heart attacks should happen within two and a half hours
When a patient experiences chest pains there's a spectrum of what could be wrong, according to Gagg.
“At the worst end of the spectrum will be a particular type of heart attack, something we call ST-elevation myocardial infarction or STEMI, because that's something which needs time critical intervention,” he said.
“Most areas will have a system that takes that patient, not through their emergency department, but directly to a coronary care unit where they can do a procedure and angiogram to release the blockage in the blood vessel that is causing the heart attack.”
Gagg told The Cornish Echo that there are national audits around making sure this treatment is received on time. He explained that 75% of patients should be having the procedure done within two and a half hours of making a telephone call.
Meeting this target would be impossible with Cornwall’s average Category 2 response time of two hours and 58 minutes.
“It's an area I know cardiologists are concerned about because they have seen delays in that time from the patient calling for an ambulance, to them being able to do the procedure, which can be lifesaving… And so that's clearly a real concern,” he said.
Response times: Bad across England, worse in Cornwall
NHS statistics show there is a problem across England with ambulance response times for conditions like heart attacks and strokes.
The national average for Category 2 calls in September this year was 47 minutes and 59 seconds - more than twice as long as the target of 18 minutes.
However, the situation in Cornwall is particularly bad.
Cornwall’s average Category 2 response time of two hours and 58 minutes was 3.8 times the national average.
Since the introduction of the Category 2 targets, the average national response time targets have rarely been met, according to the Nuffield Trust, an independent health think tank that aims to improve the quality of healthcare in the UK.
The target was first met in May 2020, when the average response time fell to 13 minutes 29 seconds.
This came alongside a fall in the number of Category 2 incidents following the onset of the Covid-19 pandemic, to a low of 323,047 incidents in May 2020 - some 16% lower than in May 2019.
Since then, Category 2 response times have gotten worse. In March 2022, the average response time was 1 hour 1 minute and 5 seconds and response times have consistently remained over double the 18 minute target time.
The human impact
Those who have had to wait a long time for ambulances have been left shaken by their experience.
The Cornish Echo spoke with Tony Clarke, an 82-year old, who lives in the village of Menheniot near Liskeard.
In June this year, he went to a hospital in Bristol to have a seven hour surgery for a Fenestrated Endovascular Aortic Aneurysm Repair.
“I had an abdominal aneurysm, which was over 60mm, which is quite big. So if you can imagine, your aorta is swollen to that dimension. If it bursts, you're dead, you lose so much blood so quickly that nobody can save you,” Tony said.
“So I had that repaired, which at my age, was quite a serious procedure.”
Following his surgery, Tony was brought home by an ambulance crew on June 18.
“My family are hundreds of miles away, all over the place. I live alone in a little sheltered council bungalow.
“I got home in the evening I think around 6pm. I didn't have anybody, I was just left in my empty house. The ambulance crew got me into bed and that was it… I didn't have any aftercare arranged at that time. There was nothing.
“Because of the nature of my operation, I had been told, quite clearly by medical staff, including the surgeon, that if I experienced any extreme or severe abdominal pain, I should dial 999 immediately… This was because the extreme pain could signify that something had gone wrong and I was bleeding. Internal bleeding from the aorta is usually extremely critical, to say the least.”
Tony Clarke feared for his life when waiting for an ambulance
That night Tony found himself experiencing agonising abdominal pain. He finally called 999 at 5.21am.
He told call handlers that he had just had surgery and reported his symptoms. They put out a Category 2 call.
But after 18 minutes he was still waiting.
“As far as I was concerned, the operation had gone wrong and I was bleeding and I was dying… I was going to die totally alone, without any family, without any friends, or even another human of any kind, with me,” he said.
An ambulance crew eventually arrived at 7.48am - two hours and 27 minutes after he had made his call.
“The crew were very concerned to find me alone and in extreme pain. They told me the call had been given Category 2 status, which obviously means that had I been bleeding internally, I would have been long gone before the arrival of the ambulance,” Tony said.
The ambulance crew stayed with Tony for more than two hours, confirming further intestinal blockages, which were the reasons for the pain. “But nobody knew that at the time,” Tony added.
Tony has had four life-threatening conditions, and he said his experience has “left a mark on him”.
“It leaves me now, hoping to God and praying that if I have another emergency, things might be better,” he said.
“If they continue at the same pace, I don't think there is much hope for people like me.”
What’s causing the delays?
A spokesperson from NHS Cornwall and Isles of Scilly Integrated Care Board, told The Cornish Echo that “operational pressures right across Cornwall’s health and care services have led to longer than acceptable waits for ambulances, ambulance handover delays and large numbers of people who are ready to leave hospitals but who are awaiting onward care or support at home”.
NHS bosses have said that a key cause of these pressures lies an inability of hospitals to discharge patients who are medically fit to leave, but who have no care package to go to.
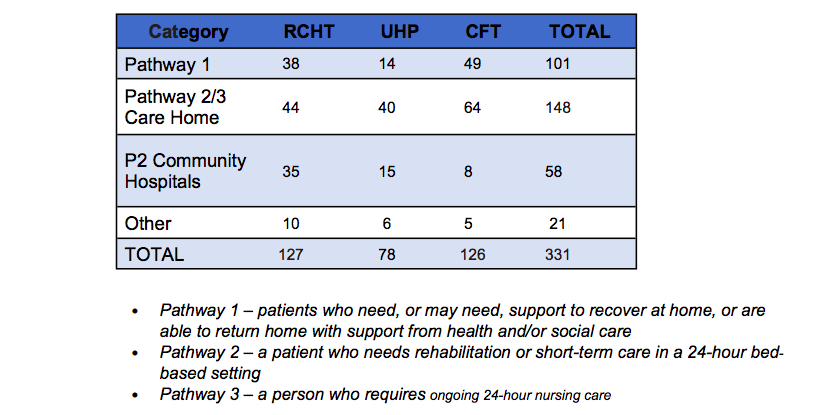
Figures from a report by RCHT's chief executive, Steve Williamson, showed that the total number of hospital beds occupied by externally delayed patients reached its highest level this year.
“Up to 14 October 2022 there had been deterioration in the number of externally delayed transfers of care for those who are medically fit but waiting for care home placements or care support packages in their own homes,” the report said.
In total, 331 beds were occupied by Cornwall and Isles of Scilly patients across the Royal Cornwall Hospital Trust, Cornwall Partnership NHS Foundation Trust (CFT) hospitals and the University Hospitals Plymouth NHS Trust Hospital.
Source: RCHT's chief executives Report to Board in Public – November 2022
“[Delays for discharges] has a consequence for the ability of the hospitals to free up bed space for people coming in the front door and the emergency department and flowing through the hospital,” explained Mario Dunn, CEO of Healthwatch Cornwall's CEO Mario Dunn.
“It has an impact on the number of ambulances that are in the system working instead of queuing up outside, and hence the number of ambulances that are available to answer emergency calls.”
The extent of the issues with flow can be seen in long ambulance handover delays, as ambulances wait until they can hand over patients to the emergency department, before getting back on the road.
Figures provided to The Cornish Echo by the NHS Cornwall and Isles of Scilly Integrated Care Board, showed that the total time lost to handover delays (waiting more than 15 minutes) at Treliske hospital for the period 1 April to 30 September 2022 was 45,425 hours.
This equates to an average of 248 hrs lost per day, or 1,738 hrs lost per week.
In the same April to September period in 2019 the trust lost 1,282 hours – this equated to an average of seven hours, or 49 hours lost per week - significantly lower than those seen within the current year.
And a Freedom of Information request sent by MP for St Ives, West Cornwall and The Isles of Scilly, Derek Thomas, found that handover times at Treliske were, at an average of five hours 16 minutes per incident, higher than the Southwest average of 43 minutes.
A spokesperson for the South Western Ambulance Service NHS Foundation Trust said: “Our ambulance clinicians strive every day to give their best to patients, but our performance has not returned to pre-pandemic levels, partly due to handover delays at emergency departments.
“Health and social care services are under enormous pressure. We are working with our partners to ensure our ambulance clinicians can get back out on the road as quickly as possible, to respond to other 999 calls within the community.”
The Department of Health and Social Care said they are providing an extra £500 million nationally to speed up discharge and free up hospital beds, reducing waits in A&E and getting ambulances back out on the road.
This is alongside NHS plans to rapidly boost capacity and resilience ahead of winter, including increasing the number of NHS 999 and 111 call handlers and creating the equivalent of at least 7,000 more beds.
“NHS England is investing an additional £150 million in ambulance trusts to support response time improvements and £20 million to upgrade the ambulance fleet, while the ambulance and support staff workforce has grown by almost 40% since April 2010,” the spokesperson added.
Care in crisis
Healthwatch Cornwall’s Dunn said that pressures in the system can be linked to a significant deterioration in Cornwall in the provision of social care services over the last few years.
“There are many factors that affect that, a lot of them have nothing to do with health and social care, but to do with practical issues like hourly wage rates, effectiveness of working in social care, availability of beds, availability of local authority support packages,” he said.
“A lot of this is peripheral for direct provision of health care, but it fundamentally affects the ability of the NHS to operate effectively.”
Dunn’s point was echoed by the Care Quality Commission’s annual State of Care Report, which was published on 21 October 2022.
The report noted that “large numbers of people are stuck in hospital longer than they need to be”, due to a lack of available social care.
“At the heart of these problems are staff shortages and struggles to recruit and retain staff right across health and care.”
Richard Monk, executive officer for Cornwall Partners in Care, a not-for-profit organisation which works to support social care providers from all sectors across Cornwall, told The Cornish Echo that it was a simple case of “you can't bring people in the front door if you can't get them out the back door”.
“There isn't enough readily available capacity in the social care sector to be able to take the number of discharges that hospitals need to achieve each day to clear the decks,” he said.
Swallowcourt, which has six care homes across Cornwall, told The Cornish Echo, that it is operating with empty beds.
“Our problem is that we don't have staff. We're constantly exploring how we can recruit more of them,” said Leah Marsh, Swallowcourt’s managing director.
“We're quite good at retaining staff, but obviously when an Aldi opens up down the road and they're paying £11.50 an hour, even as a foundation living wage employer, we're struggling to pay £10 an hour, where would people rather go and work?
“We can bring in people from out of the county to come and work for us. But where are they going to live?”
Marsh said that the biggest stumbling block for her organisation is a lack of affordable accommodation to bring in either overseas staff or staff from outside of Cornwall.
“If we don't get paid enough for the care that we provide, we can't pay our staff enough money to grow it to be an attractive proposition. And without any affordable accommodation to support this, we accept that we are contributing to a blockage,” she added.
Rising costs due to inflationary pressures make it harder to increase salaries for potential care staff, which might attract them into the job.
Marsh said that back in April they received a 2.8% inflation increase from the local authority on care fees.
“Since that time, energy costs have rocketed, they've gone through the roof, and we have big buildings that need to have the heating and the lights on. We're caring for elderly people. These homes need to be warm and well-lit,” she said.
And a funding uplift due in April is unlikely to cover the cost, according to Cornwall Partners in Care's Monk.
“I would imagine that when Cornwall Council comes to their decision as to what the uplift for care providers will be from April of next year, it'll probably be 2% to 3% or something like that. It won’t be enough.”
He told of one small care home, with less than 20 beds, whose fuel bill went from about £4,700 a year to £22,000 a year.
“There's no meat left on the bone. If we got any kind of fee uplift right now, it would go straight to our teams,” said Marsh.
“I mean, we're looking at operating voluntary food banks in our homes because we know that some of our team members are struggling. We do have within staff rooms, pasta and tins of food, that people can just take out. We shouldn't have to do this. These guys are working their backsides off… We should be paying a wage that's comparable to stacking a shelf.”
Care providers in Cornwall were recently asked to detail their costs as part of the government’s fair cost of care policy, which examines the practice of councils paying providers fees that do not adequately cover costs.
“The government now knows how much it costs to provide care. Are they going to be willing to put their hands in their pockets and pay for it? How big are their pockets?” said Monk.
A spokesperson for Cornwall Council said it is part of the Proud to Care Cornwall initiative that aims to bring more workers into Cornwall’s care sector.
It brings together care providers from across Cornwall who provide each other with support as well as all working together to promote care sector roles and advertise job vacancies across the care provider market.
The council also ensures that the care that they commission pays workers at least the foundation living wage.
“We are also a member of Association of Directors of Adult Social Services who are campaigning for care workers’ pay to be in line with NHS workers.
“It is hoped that government funding for this initiative will come through investment in social care reforms that is expected in April 2023,” the spokesperson added.
What’s being done?
The report presented by RCHT's chief executive, Steve Williamson to Cornwall’s integrated care board, said that “significant work” has been undertaken since mid-October with community and voluntary sector partners to increase community capacity to support the discharge of patients waiting to go home who require some community care (pathway 1 patients who don’t need as much care).
“This has resulted in a significant reduction in the number of P1 patients in RCHT which reduced to 14 on 26 October 2022,” the report said.
RCHT said it has also taken a comprehensive range of actions to address the issues impacting on ambulance handover delays.
These include a RCHT Flow program to transform acute hospital flow management, capacity and performance and the relocation and establishment of the discharge lounge as an ambulatory facility to improve access and prevent the space from being bedded.
RCHT’s urgent and emergency care teams are being supported by the NHS Emergency Care Intensive Support Team and the South West Urgent and Emergency Care Team through an “intensive focus week” at the start of November, which will also involve community hospitals and teams at Cornwall Partnership Foundation NHS Trust.
“This will then lead into a ‘reset’ period, as part of our Flow Programme, where we aim to achieve a sustained reduction in the pressure centred on our hospitals,” the report said.
The Cornish Echo approached all of Cornwall’s MPs for comment.
St Ives, West Cornwall and the Isles of Scilly MP, Derek Thomas, said: “I’ve been pushing for action on the flow of patients at Treliske – meeting ministers and officials from the Department for Health and Social Care in Whitehall to demand action, and seeking answers from regional commissioners, hospitals and all the different bodies providing social care.”
Thomas added that the ambulance delays in Cornwall are “clearly not acceptable” and that “lives have been lost” because ambulances are not getting to incidents in time.
“Each individual delay causes distress and anxiety, but it’s clear from my investigations that there is a failure of the whole system of health and social care – admissions into A&E are where this failure is clearest,” he added.